Research
Radiology, nuclear medicine and medical imaging at University of Toronto was ranked in the top 10 research departments in the world by the 2021 U.S. News & World Report.
Dr. Sangeet Ghai
Research, Activity Lead
publications/year in peer-reviewed journals
of high impact journals with the JDMI members as Principal Author or Senior Responsible Author in 2020
per year: the average citation score for the Clinician Scientists
the average total number of citations per year for the department
About
The Joint Department of Medical Imaging is the largest radiology department within the University of Toronto with over 70 FTEs providing clinical care, radiology residency training to the future generation and also achieving academic laurels for the institute.
There are 10 Clinician-Scientists in the department who devote most of their time to research. The Scientists have successful funding to support their research activities and the institute recognizes the important research contributions made by these Principal Investigators. Other staff have appointments as Clinician Investigators at one of the four research institutes at UHN.
JDMI radiologists and in particular Clinician-Scientists have been successful in securing peer-reviewed grant funding, including CIHR grants, PSI, OICR, Heart & Stroke foundation, and Prostate Cancer Canada to name a few. Many of the PIs hold in excess of $4-5M in grants. The department also holds two research chair positions at University of Toronto.
JDMI also takes pride in many “first” research achievements, some of which are now completing Phase II/III trials and are likely to be ready for clinical approval across the globe in the next year or two.
Our Work
The existing infrastructure provides a fertile ground for research led by the Division’s staff and trainees. Two of our staff have protected research time through the JDMI Research Leadership awards. Between January 2018 and December 2020, members of the division have published over 70 manuscripts in peer reviewed journals and have presented their work in the leading society meetings (Society of Nuclear Medicine & Molecular Imaging, European Society of Nuclear Medicine, Radiological Society of North America, and the American Roentgen Ray Society annual meetings among others.
There are currently more than 30 research projects ongoing in Molecular Imaging. Research projects in PET/CT and PET/MR span wide areas in imaging-based oncology research including prostate cancer, sarcomas, lung cancer, breast cancer, liver cancer, esophageal cancer, H&N as well as gynecological diseases. Furthermore, non-oncological indications like transplant graft evaluation, peripheral artery disease and rheumatoid arthritis are being investigated.
Cardio-vascular research, dedicated MSK projects and also an array of PET-based and MR-based technical research is being conducted in the context of hybrid imaging. Molecular Imaging has well established co-operations on different levels of research directly with headquarters of the vendors were are working with.
Consecutively, joint projects are being carried out continuously and the division has a successful track record of attracting industry as well as competitive research funding.
Research
Select a Division below to learn more about our research.
Divisions
The Prostate Evaluation for Clinically Important Disease: MRI vs Standard Evaluation Procedures (PRECISE) study
Dr. Masoom Haider was the co-PI on PRECISE, a large multicenter Canadian trial investigating the use of MRI for prostate cancer diagnosis.
The findings published in JAMA Oncology showed that MRI together with targeted biopsies offer patients a less invasive procedure for prostate cancer diagnostics and even the chance to avoid a biopsy altogether while detecting clinically significant cancers.
As a result, a revised guideline for Ontario patients was issued earlier this year with a recommendation that all men at risk for prostate cancer have an MRI – practice that is now covered under OHIP, replacing the previous standard of care where all male patients with an abnormal PSA test were referred for a biopsy.
A formal 2-year follow up will be performed on all patients who participated in the study.
Federated learning for predicting clinical outcomes in patients with COVID-19
 The objective of this study published in Nature Medicine was to develop a robust, generalizable federated learning (FL) model that could assist in triaging COVID-19 patients, predicting their future oxygen requirements.
The objective of this study published in Nature Medicine was to develop a robust, generalizable federated learning (FL) model that could assist in triaging COVID-19 patients, predicting their future oxygen requirements.
Federated learning is a machine learning technique that trains an algorithm across multiple servers holding local data, without exchanging them, which alleviates any privacy concerns and removes barriers to data sharing.
BREAST
The breast division has an array of stellar research faculty working on a wide variety of research projects, international trials and collaborations. Through engaging in collaborative clinical trials, the divisional members have strived to develop new technologies for the early detection of breast cancer, which push forward precision and personalized medicine, benefiting both the average and high-risk patients. Some of our key research initiatives and researchers are highlighted here:
- TMIST Trial, comparing digital breast tomosynthesis versus digital mammography for screening. MSH-UHN sites are soon looking to onboard the TMIST trial spearheaded by Dr. Vivianne Freitas, who will be the Principal Investigator.
- Dr Vivianne Freitas is working on a collaborative prospective clinical trial with Lakehead University, Thunder Bay, ON, Canada, which aims to evaluate a novel Positron Emission Mammography (R-PEM) device, entirely developed in Canada that may emerge as a promising new imaging tool for the detection of breast cancer.
- Breast Imaging projects in artificial intelligence are underway in the led by Dr. Vivianne Freitas in collaboration with the Sinai Radiomics and Oncology Research Laboratory, lead Dr. Massom Haider.
- Dr. Anabel Scaranelo leads revolutionary research exploring non contrast techniques in breast MRI for breast cancer diagnosis via diffusion-tensor imaging (DTI) in collaboration with Dr. Hadassa Degani from the Weizmann Institute of Science, Israel.
Multiple other clinical research projects initiated by breast radiologists continue at each site along with mandatory annual fellow research projects as well as multidisciplinary research collaborations.
CARDIOTHORACIC
Clinical Utility of New Cardiovascular Imaging Techniques
The overarching goal of this program is to evaluate the clinical utility of new cardiovascular imaging techniques including diagnostic certainty, prognostic value, healthcare utilization, and cost effectiveness.
The results of these studies provide a rationale for integrating these new techniques into clinical practice, including T1/T2 parametric mapping and cardiac PET/MRI.

Role of Multi-Parametric Cardiac MRI in Identifying Myocardial Damage
The aim of this research program is to establish the role of quantitative cardiac MRI parametric mapping in the evaluation of myocardial damage. Current projects are focused on the evaluation of myocardial damage in patients with rheumatologic diseases, in patients who have recently recovered from COVID-19, and patients with myocarditis after COVID-19 vaccination.
Patients are currently being recruited for advanced cardiac imaging after COVID-19 and COVID-19 vaccination to evaluate the prevalence and pattern of myocardial damage with initial results expected end of 2021.
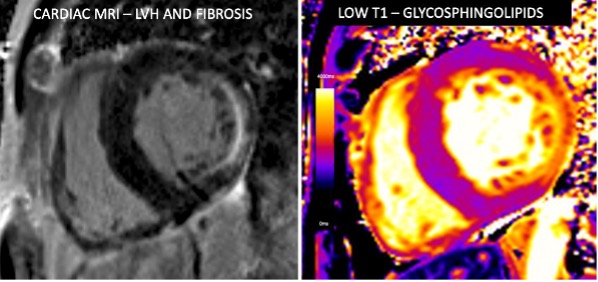
Diagnostic and Prognostic Significance of Cardiac MRI in Fabry Disease
One of Dr. Hanneman’s most significant contributions to the field of cardiac imaging over the past five years has been in demonstrating the role of cardiac MRI in detecting early cardiac involvement, monitoring disease progression, and stratifying risk in patients with Fabry disease. On-going studies are evaluating longitudinal changes in MRI parameters in relation to treatment status.
Dr. Hanneman has recently launched a large international multi-center prospective cohort study funded by CIHR which will enroll 250 Fabry patients from nine Canadian and international sites. The overarching goal is to identify early cardiac abnormalities in high-risk Fabry patients non-invasively using multiparametric cardiac MRI T1/T2 mapping and blood biomarkers to guide treatment decisions and improve patient outcomes.
Dr. Hanneman has published seven manuscripts to date as senior author based on this body of work. The results of this work have been cited in national treatment guidelines and have directly influenced management of patients with Fabry cardiomyopathy by providing a rationale for the role of cardiac MRI in investigating patients with suspected Fabry cardiomyopathy and guiding treatment decisions.
Dr. Micheal McInnis
Iodine Subtraction Chest CT Pulmonary Angiogram
The Toronto General Hospital Chronic Thromboembolic Pulmonary Hypertension (CTEPH) Team evaluates patients from across Canada. CTEPH is caused by chronic blood clots in the lungs and, if left untreated, the prognosis is poor.
Pulmonary endarterectomy is the gold standard treatment for CTEPH and, prior to surgery, we perform state-of-the-art iodine subtraction computed tomography (CT) pulmonary angiography. Our research use of high-quality CT has helped us better understand the imaging findings in relation to the surgery and the expected patient outcomes.
In partnership with Altis Labs Inc. and with a multidisciplinary team from UHN, Dr. Felipe S. Torres is working on developing AI models to evaluate patients with lung cancer and those with lung infection. The goal is to develop an image-based prognostication tool using deep learning that could provide personalized information to guide treatment and monitoring decisions.
Dr. Gauri Rani Karur
Cardiac MRI biomarkers of myocardial remodeling and genotype-phenotype correlations in hereditary thoracic aortic disorders
($35,250 / one-year award by GADA Canada as part of its Research Grant Award program)
Recent studies have suggested that there may be subtle abnormalities of the heart muscle in addition to the well-known abnormalities of the aorta and the heart valves in hereditary thoracic aortic disorders (HTAD).
This study will perform a detailed MRI evaluation of the heart to compare HTAD patients to healthy control volunteers and HTAD patients treated with beta-blockers (BB) and angiotensin-II receptor blockers (ARB) to those who are not.
Interventional Radiology
TVA Medical: Endovascular Dialysis Fistula Creation Device
The first case of endovascular dialysis fistula creation was performed by Dr. Dheeraj Rajan in 2012 with a device created by TVA Medical. This was part of an initial first-in-human feasibility study that today has led to global adoption of this technology.
Dermaport: Titanium Hub for Dialysis Catheters
The first-in-human study was initiated at Toronto General Hospital in 2008. The technology involves a unique titanium mesh that acts as a barrier to infection for tunneled dialysis catheters while facilitating catheter repositioning and exchanges.
Vascular Medcure: Novel Thrombectomy Device for Thrombosed Dialysis Grafts
We are currently conducting a first in human study to assess safety and efficacy of a novel thrombectomy device for thrombosed dialysis grafts. The device, unlike other devices, does not have an aspiration component and does not require use of lytics.
A Prospective, Single-Centre Study Investigating the Clinical Use and Safety of the Jetstream Atherectomy with Drug Coated Balloon (Ranger) for the Treatment of Dysfunctional Arterio-Venous Graft Stenosis.
Peter Munk Cardiac Centre Innovation Fund, University Health Network. 58,800 CAD
February 2021 – February 2023
Principal Investigator
This single-centre, single-arm, prospective study will enroll 30 subjects with clinical and hemodynamic abnormalities in arteriovenous graft (AVG) in the arm. Subjects will be treated with the Jetstream™ atherectomy device and Ranger™ Drug Coated Balloons (DCB) and followed up clinically in an-office visit or via phone at six and 12 months post-procedure.
This study is to demonstrate safety and assess the clinical use and outcomes of the Jetstream ™atherectomy device and Ranger™ DCB for the treatment of dysfunctional AV graft.
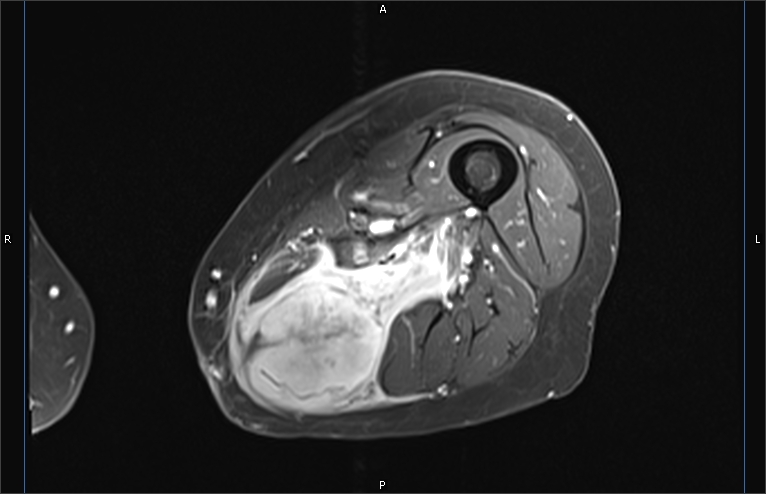
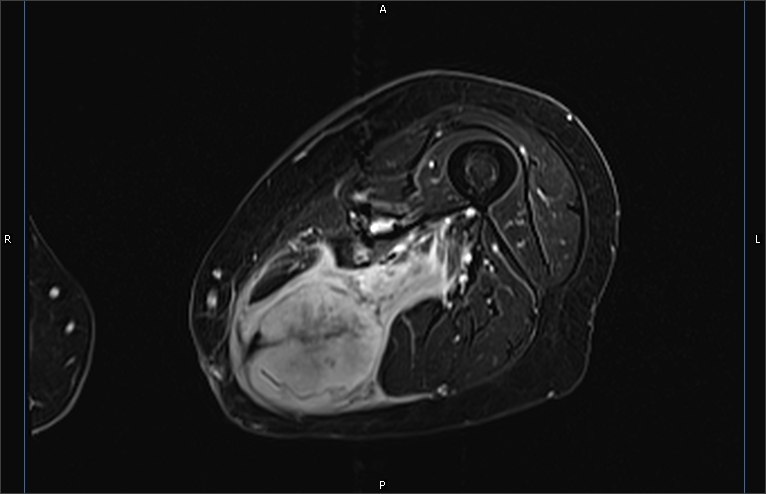
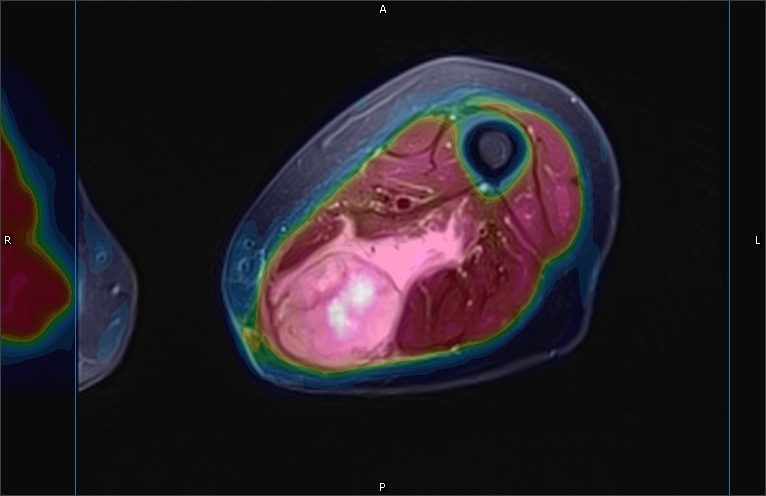
Evaluation of Prognostic Value of 18f-Fluoroazomycin Arabinoside (FAZA)
2019 Aug – 2021 Aug
Co-Investigator
Positron Emission Tomography/Magnetic Resonance Imaging (PET/MR) In Patients with Critical Limb Ischemia pre- and post Revascularization: A Pilot Study.
Joint Department of Medical Imaging Academic Incentive Fund, University Health Network.
PI: Dr. Patrick Veit-Haibach. 40,000 CAD
Peripheral artery disease is a worldwide problem that leads to high mortality and morbidity.
Critical limb ischemia (CLI) is associated with a high risk of amputation and the subsequent decreased quality of life. Endovascular therapy is now considered the primary treatment option in these patients to improve the vascularity and prevent amputations.
In recent years, molecular imaging tools have become available. A recent radio tracer 18F-Fluoroazomycin Arabinoside (FAZA) is a specific marker of hypoxia in the tissues and has been used in multiple studies. This tracer can be used in PET/MR scan and present itself as a potentially powerful diagnostic tool in patients with CLI. In one diagnostic study, it allowed for the evaluation of location and degree of hypoxia in the extremity tissues. This diagnostic tool may offer a better assessment pre- and post-standard-of-care endovascular treatment for the patients.
Some of the patients treated with endovascular therapy may not have a favourable outcome, and we don’t yet have a clear understanding of why this happens. We will try to find some predictor model in the FAZA PET/MR that can explain the different outcomes and may help clinicians choose the best treatment option in specific cases.
Thirdly, post-processing for optimization of the MR sequences in patients with CLI will be performed at the MR component of the PET. There would be a great clinical interest in developing non-invasive tools that could provide more accurate diagnostic information compared to traditional tests for the above patient populations.
Comparison of Carbon Dioxide Flush and Saline Flush to Saline Flush Alone in TEVAR and TAVI Procedures to Reduce Cerebral Ischemia.
Peter Munk Cardiac Centre Innovation Fund, University Health Network. 50,000 CAD
2019 Jun – 2020 Jul Principal Investigator.
Thoracic endovascular repair (TEVAR) and transcatheter aortic valve implantation (TAVI) are the standard-of-care procedures to treat thoracic aortic aneurysm or severe aortic stenosis, respectively. Both procedures have a high risk of stroke and silent infarction.
Gas has been detected in the cerebral vasculature during these procedures and associated with DWI positive lesions on MRI. The hypothesis is that air emboli contribute to stroke and silent infarction. The investigators propose addressing air emboli by flushing the device with carbon dioxide prior to flushing with saline. This is a pilot study comparing standard saline flush alone to carbon dioxide flushing with saline flush.
MOLECULAR IMAGING
 PSMA-Targeted PET in the Clinical Care Paths
PSMA-Targeted PET in the Clinical Care Paths
Prostate-specific membrane antigen (PSMA)-targeted positron emission tomography (PET) is increasingly being used worldwide as part of the clinical workup for men with prostate cancer. With high overall accuracy for the detection of prostate cancer, PSMA-targeted PET has an increasingly established role in the setting of biochemical failure after primary therapy. This best practice report suggests current indications for PSMA-targeted PET in the clinical care paths in the Canadian context.
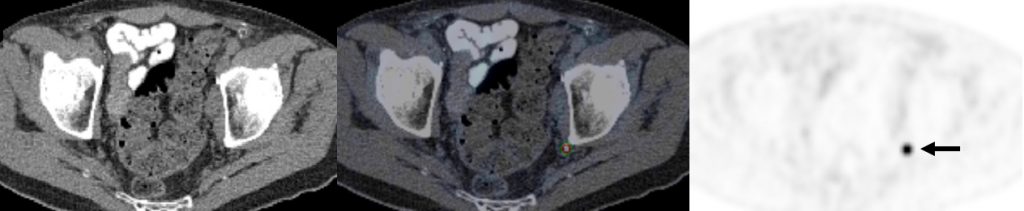
78-year-old man 4 years after radical prostatectomy for pT3a N0 adenocarcinoma of prostate ISUP Grade Group 3. Now biochemical recurrence (serum PSA = 0.80 ng/ml); PET performed prior to salvage prostate bed radiotherapy. (A) MIP PET image showing solitary focus of abnormal tracer uptake in the pelvis on the left. (B) Axial PET/CT image (CT – left; fused PET/CT – middle; PET – right) shows an intensely 18F-DCFPyL-avid 0.3 cm left pelvic sidewall lymph node (SUVmax = 25.6; PSMA score, 3), in keeping with a metastatic node. After PET, the patient was treated PET-directed stereotactic radiotherapy with favorable metabolic response.
The impact of 18F-DCFPyL PET/CT on the management of patients with recurrent prostate cancer: Results of a Prospective, Multicenter Trial
This study was accepted for presentation at the RSNA meeting 2021 (Nov 28, 2021- Dec 2, 2021; Chicago, Il, USA). It was also chosen as one of three studies to be highlighted in the RSNA Best Clinical Trials session of the meeting.
PSMA-PET detects additional sites of disease compared with standard of care imaging in most men with biochemical failure and suspected low volume metastatic disease, resulting in frequent change in management including a change from palliative to curative/radical intent therapy in 20% of men.
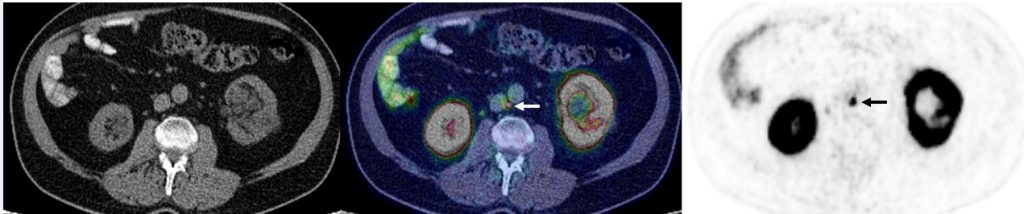
71-year-old man with biochemical recurrence of prostate cancer (PSA = 0.17 ng/ml) following radical prostatectomy and pelvic salvage radiotherapy. PSMA PET/CT shows single metastatic 0.3 cm interaortocaval lymph node, confirming disease recurrence.

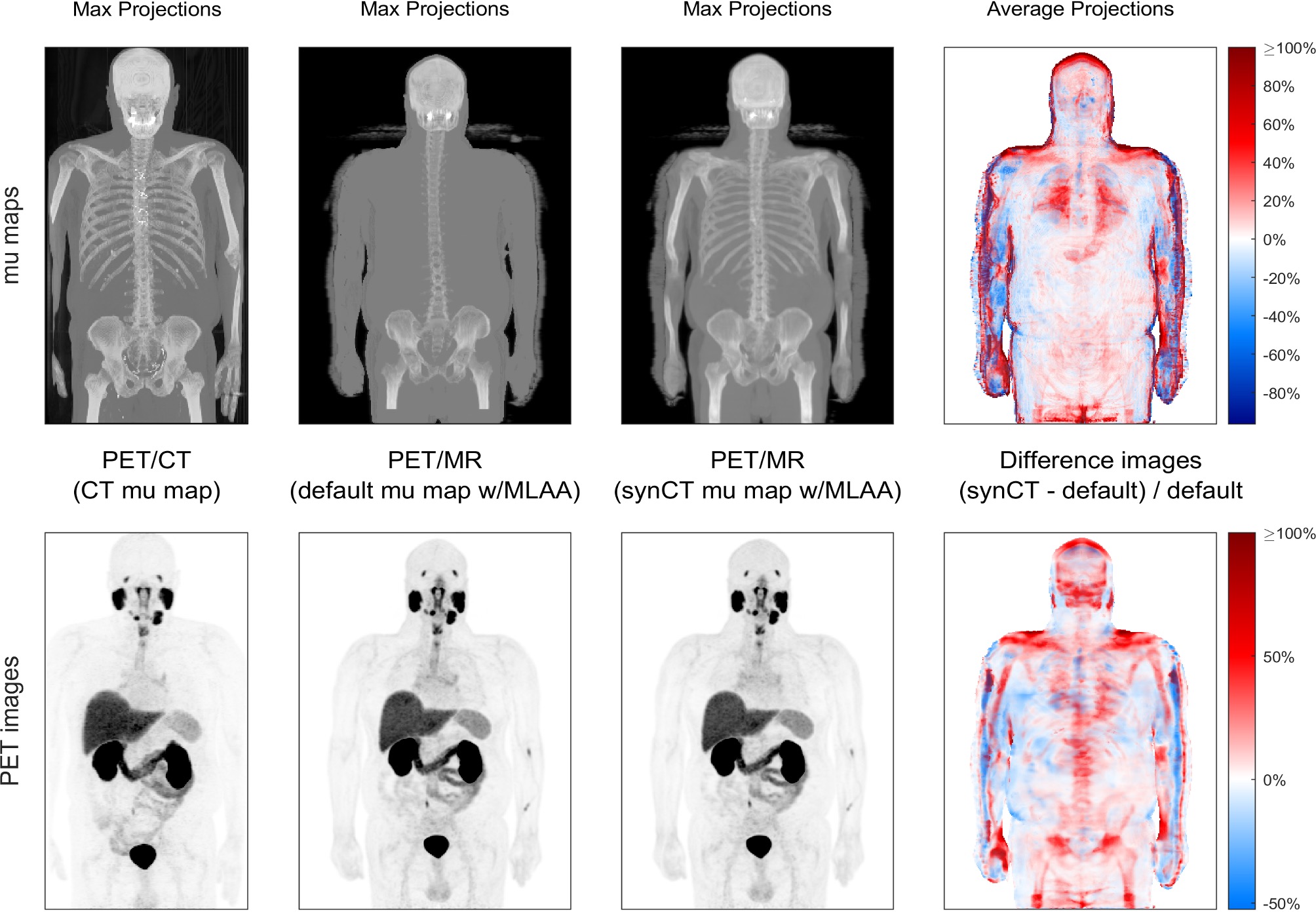
Dr. Patrick Veit-Haibach is an active researcher with several research interests and projects in hybrid imaging, image quality improvement, and radiomics methods.
For hybrid imaging, he researches ways to evaluate metabolic, morphological, and functional changes in tumours and cardiovascular diseases through the use of CT, MRI, and PET (including novel tracer deployment and use).
Dr. Veit-Haibach is also engaged in research focused on motion correction to improve image quantification. Although patients are asked to remain still for many imaging procedures, some physiological processes, such as breathing, are impossible to suppress for a long time, which leads to artifacts on the images. Dr. Veit-Haibach and his colleagues are working on technologies to correct for such motions.
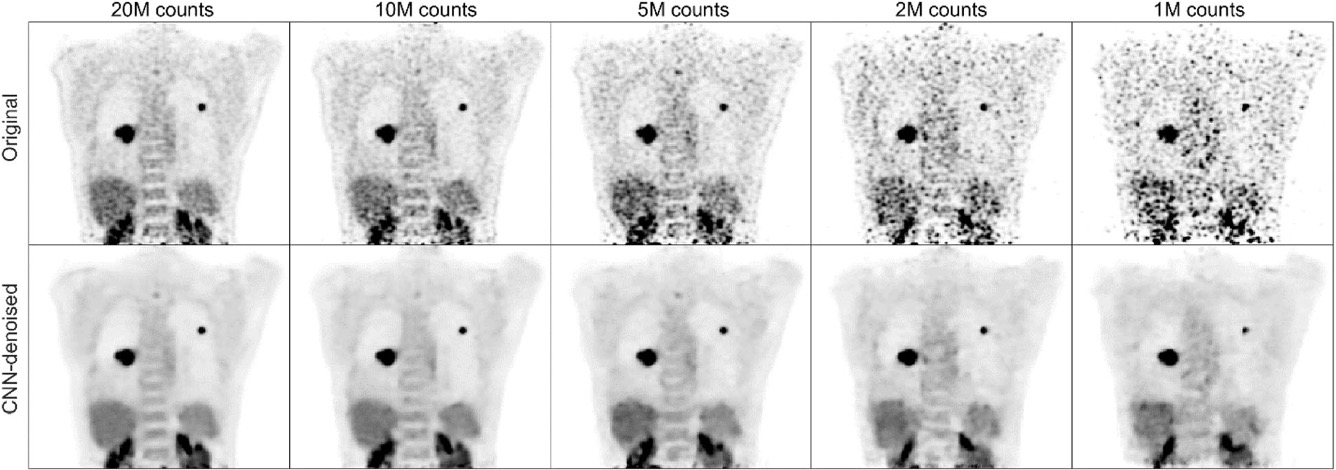
Veit-Haibach’s research on improving image quality also includes methods to quantify biological readouts in PET, and ways of improving attenuation correction required for every PET image.
Dr. Veit-Haibach research in dynamic PET imaging allows for a better differentiation of certain processes which we are often present in images (such as areas that show no clear distinction between an inflammation and a reaction to therapy).
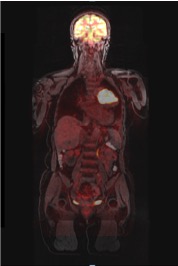
His research interest also lies in gastroesophageal cancer and sarcoma.
Dr. Veit-Haibach is also a member of the Hypoxia Imaging Program, which brings together interventional radiologists and kidney transplant clinicians to identify hypoxic states in tumors in vascular imaging.
Radiogenomics
Radiomics is a technique that uses algorithms and data processing to extract quantitative features from PET, CT, and MRI images. These radiomics features can then be correlated with other variables, such as patient outcomes. In radiogenomics, the radiomics features are compared with the underlying genomics. Research in this field may allow scientists to harness the power of both imaging and genomics to predict a cancer patient’s response to treatment or prognosis.
Neuroradiology
MRI screening to identify silent strokes in real-time and prevent dementia
More than half of adults over the age of 65 have injuries in the nerve fibers (white matter) of the brain. While these injuries may be left unnoticed early on, as they worsen with time, they can impair mental abilities and cause dementia. These injuries are a problem on their own (vascular dementia), and can also worsen the symptoms of Alzheimer’s disease.
These nerve fiber injuries are caused by disease of the small blood vessels in the brain. The challenge is that nerve fiber injury occurs irregularly over time. While we can use MRI scanning to see old nerve fiber injuries, we don’t have a way of identifying active, ongoing damage that we can try to halt.
Our Previous Work
Previous research from our group suggests that at least some of the nerve fiber injuries are due to tiny strokes. Each stroke may be small enough to be unnoticed. Such silent strokes may accumulate over the years and affect mental abilities.
A challenge of developing treatments to prevent or slow these injuries is that they develop slowly, over many years. Research studies of possible treatments require long periods of time to see if the treatment is effective. Another challenge is that these injuries often occur irregularly over time, and treatment is more likely to be useful when it is applied during a period when there is an active, ongoing injury.
Our Current Project
We are currently leading a project called “Acute Microinfarcts as a Biomarker of Cerebral Small Vessel Disease.” The project is funded by a 3-year grant from the Heart and Stroke Foundation of Canada. The goal of the project is to determine whether MRI scanning of the brain to identify tiny silent strokes in real-time provides a way of identifying people who are having active disease in the small blood vessels, and to determine if this active disease eventually leads to impairment of mental abilities. We are using a newly developed MRI scanning technique that provides vastly improved resolution compared with previous scanning techniques. This should allow us to detect very small silent strokes, potentially identifying those people who are having silent strokes using a single 10-minute scan.
If we can identify people who are having active, ongoing injuries in the white matter of the brain, then we can use this scanning technique to select participants for clinical trials of treatments to slow or halt the white matter injuries. This scanning technique could also be used to determine how well the treatment is working. The study is actively recruiting participants.
Intracranial blood vessel wall MRI: redefining the diagnostic work-up of stroke
After someone has had a stroke, doctors need to determine its cause to select the treatment that will prevent another stroke from occurring. The challenge is that conventional medical tests do not find the cause in one out of every four strokes.
People who have had a stroke usually have a scan to determine if there is narrowing of the blood vessels which supply blood to the brain. In some cases, the blood vessels are not narrowed so the test result is normal, but there is an undetected disease inside the wall of the blood vessel. Our research team has had a leading role in using high-resolution magnetic resonance imaging (MRI) to assess the blood vessel wall. This “intracranial blood vessel wall MRI” can identify the cause of a stroke in cases where the cause was previously unclear.
Some of our original contributions to this field are:
- Use of blood vessel wall MRI to distinguish between blood vessel constriction and blood vessel inflammation
- Use of blood vessel wall MRI to assess brain aneurysms
- Use of blood vessel wall MRI to assess vessel wall injury after stroke treatment
- Use of blood vessel wall MRI to distinguish between stable and unstable atherosclerotic plaque
- Determining the impact of using blood vessel wall MRI in people who have a stroke of unclear cause
- A clinical practice guideline on use of blood vessel wall MRI
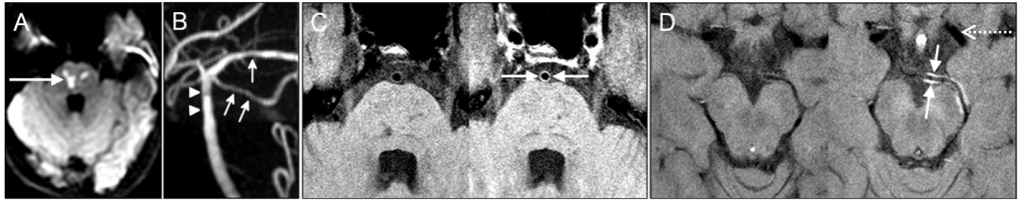
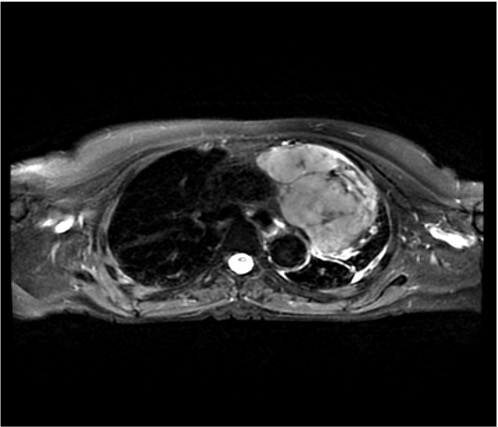
EXAMPLE. Young man with headache, nausea, and double vision. MRI of the brain shows sudden-onset stroke in the brainstem (arrow in A). There is mild narrowing of blood vessels supplying this part of the brain (arrows/arrowheads in B). High-resolution blood vessel wall MRI (C, D) was performed at the Toronto Western Hospital. The images obtained before and after intravenous injection of contrast material (left and right side of each pair, respecitvely) show uptake of contrast material into the blood vessel wall (arrows in C and D) consistent with inflammation in the blood vessel wall. The vessel wall imaging helped confirm the diagnosis of vasculitis and brain biopsy was avoided. There is a normal blood vessel (dotted arrow in D) for comparison.